Closure of Skin for Optimal Cosmesis
Skin Closure

At the end of the day, apart from functionality, the two things that bother the patient are the bulge of the pocket and scar of the incision – both are at the mercy of the operator
Introduction
The role of skin suture is to heal the dermal gap to seal off the wound. Provided that the second layer of the sub-cutaneous tissues were properly sutured, the tension on the skin edges would be minimal. Hence skin suturing pacing has only a minimal role to play with regard to wound security. However the sutures do play a vital role in environmentally sealing the pocket until deep tissues are healed. The other factor is the need for cosmesis and therefore a minimalist approach is necessary to minimize suture material while maintaining adequate security and sealing.
Cosmetic Concerns
Young patients & female patients may have significant concerns with regard to cosmesis. All implantations should be cosmetically sound but when there is particular significance, then pre planning is essential. If the operator is experienced, a totally different pocket (e.g. in the sub-mammary space) can be considered. Regardless of operator experience its always better to use the standard place to implant as future box changes may become complicated in non-standard locations. With meticulous technique, most pacemakers can be implanted in seemingly “invisible” pockets in the standard location. ICDs may be a concern as the device bulk is greater
Suture Material
Non – absorbable suture materials give the best scar – as they can be completely removed after 7 days. Absorbable materials (e.g Vicryl, Monocryl and Dexxon) may leave residual material even after 7 days as the removal may be partial. Although modern absorbable material have minimal reaction, it is not zero and any left over can lead to scar enlargement
In addition, if there is a chance of infection (e.g Following box change or lead replacement) its’ always better to use non-absorable material – preferably a fiber-less material such as prolene. Silk is also acceptable provided the sutures are removed within 7 days.
Suture materials : Commonly used materials are Vicryl, Monocryl, Prolene and Silk. Again as physical security is trumped by cosmesis, we use 3/0 thickness as maximum allowed. If available we may use thinner material (e.g 4/0 or 5/0) as they are equally efficient in keeping the dermal edges approximated at lesser suture bulk.
Type of Suture and Needles
Type of stitch depends on the operator’s preference. I frequently try to use sub-cuticular suture as the cosmetic outcome is excellent. From a maerials point of view – Prolene and Monocryl are the best for subcuticular sutures. Vicryl also can be used but Silk is not recommended for subcuticular sutures as the fibers may break and retain inside with subsequent infection
The type of stitch determines the needle that is used. Straight needles are the easiest to use for sub-cuticular suture although curved needles are also acceptable. Curved needles take time to be applied in sub-cuticular fashion.
For interrupted sutures, thinnest possible (3/0 or 4/o) silk or prolene is used. Ideally the needles should be reverse cutting to minimize skin damage.
From handling point of view, 4/0 silk is the best for interrupted. . Vicryl should not be used on skin as interrupted as it can break up during healing leading to retained segments. Silk has excellent knotting and friction characteristics and therefore is them most easiest to apply as interrupted sutures with good cosmetic outcome. If there is a risk of infection (e.g box changes, after complicate pocket procedure) then Prolene can be used as the suture material. Due to in its slippery nature, Prolene has poor knotting characteristics and precise knotting (surgeon’s knot) is necessary for security.
From a wound security point of view, any suture technique would be sufficient to hold the skin together until healing occurs as this region is under low tension. Therefore the suture technique directly affects cosmesis rather than wound integrity.
Default preference is for the sub-cuticular suture. However at times interrupted sutures may be required. For For example, an emaciated patient with minimal tissue flaps would benefit from interrupted sutures to ensure wound security. Another instance would be bleeding tendency where a there is possibility of forming a collection in sub-cutaneous or pocket tissues : where interrupted stitches would permit fluid to escape.
If interrupted stitches are applied, they should be evenly applied simple interrupted sutures and NOT mattress sutures. Mattress sutures can create unsightly scars whereas simple sutures leave minimal scar. If one has to resort to mattress sutures, then there is something wrong in the pocket where undue tension is needed for closure.
Sub-cuticular Suture
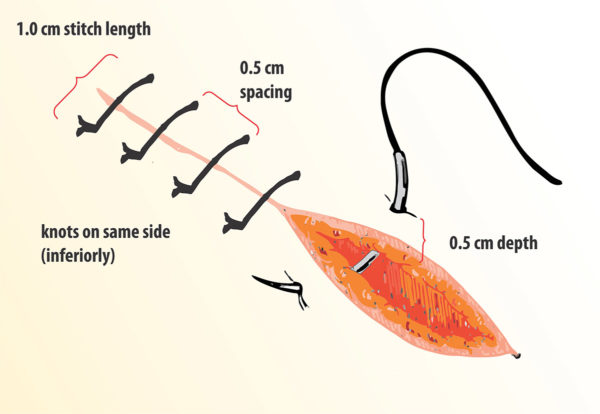
A handheld straight needle is the easiest way to apply this suture. As shown in the video, the bites should be closely spaced and taken within the dermal substance. Close spacing of bites ensure that no gaps are left. The depth of the bite (i.e. from the skin surface) should be equal on both side to ensure that there is no overlapping after suturing.
The ends can be either totally buried or as demonstrated free form. The totally buried form is convenient for the patient as there is no need for suture removal – but the author has seen two cases where the buried ends led to stitch abscess requiring wound exploration to remove the end knots. The author is paranoid about infections and therefore prefers to remove all sutures by day 7. The free form variety helps as one can remove the thread from one end at day 7.
Video : Subcuticular Suture using vicryl 3/0, straight needle. The bites are taken in even spacing, just beneath the dermis.
Interrupted Suture
Interrupted sutures provide very robust wound closure at a slight (note : slight) expense of cosmesis. In practice, unless the patient has hypetrophied scarring tendency or the technique is poor, the cosmetic outcome is near similar to subcuticular suture. Situations where interrupted sutures may be preferable
- Skin under tension from a large device : This should not be undue tension from an inadequate pocket. Most ICD pockets can be closed with sub-cuticular suture with zero tension provided the pocket is adeuqte. However in thin subjects, there may be some tension on the incision line and interrupted sutures may give better wound security
- Complicated pocket : e.g. reopened pocket due to dislodged lead or hematoma, after pocket revision to prevent an erosion, prolonged and complicated lead upgrade or lead related procedure where the pocket needed revision, Uneven pocket edges from poor incision technique etc…
If interrupted sutures are applied, 4/0 silk (on a reverse cutting curve needle) is the best as it has excellent knotting and handling characteristics.
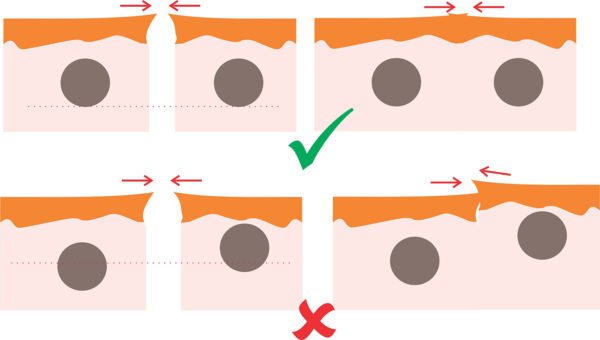
In application of interrupted suture, the individual stitches should be evenly spaced and of adequate depth extending up to the upper layer (second layer ) of the pocket closure. The lateral spacing to the stitches should be around 4 to 5 mm on either side of the wound edge. The inter suture spacing should be around 5 mm and leaving large gaps between each suture should be avoided as the spaces could gape.
The sutures should be just sufficient to keep the wound edges approximated and not too tight. Even slightest of skin wrinkling suggest a too – tight suture and these should be removed and re-applied. Tightness of the suture directly correlates with the scar becoming like a caterpillar and this should not happen. The knot it self is a simple granny knot. If properly knotted, one knot is enough for silk.
Video : Interrupted suture – Black Silk
Before applying the suture we used to clean the wound edges with povidone iodine – But that step may be unnecessary as we any way keep a povidone iodine swab over the wound before application of dressing. We don’t’ have access to water proof transparent materials to cover the wound. Pacemakers are expensive devices and infection can be disastrous – therefore we do not advocate wetting of the device pocket until all sutures have been removed and the wound inspected after 7 days of implantation.
The patient can get a head bath / sponging / body wash without wetting the wound and our patients have devised remarkable ways to do so. Although it’s a bit inconvenient from the patient’s perspective, preventing a device infection outweighs this little inconvenience. Although evidence from other surgical site wounds in general surgery have indicated that early bathing has no increased infection rate, we are paranoid of our devices and take all precautionary measures to avoid an infection. This protocol of 7 days of no disturbance has had remarkable success with regard to minimizing short term (1 year) wound complications for nearly half a decade at the authors’ institution.