Basic anatomical concepts of creating a pocket for a pacemaker in the pectoral region
Anatomical Considerations for Creating the Pacemaker Pocket
Overview
Sound knowledge of regional anatomy is essential for long-term success (minimize complications) in cardiac pacing
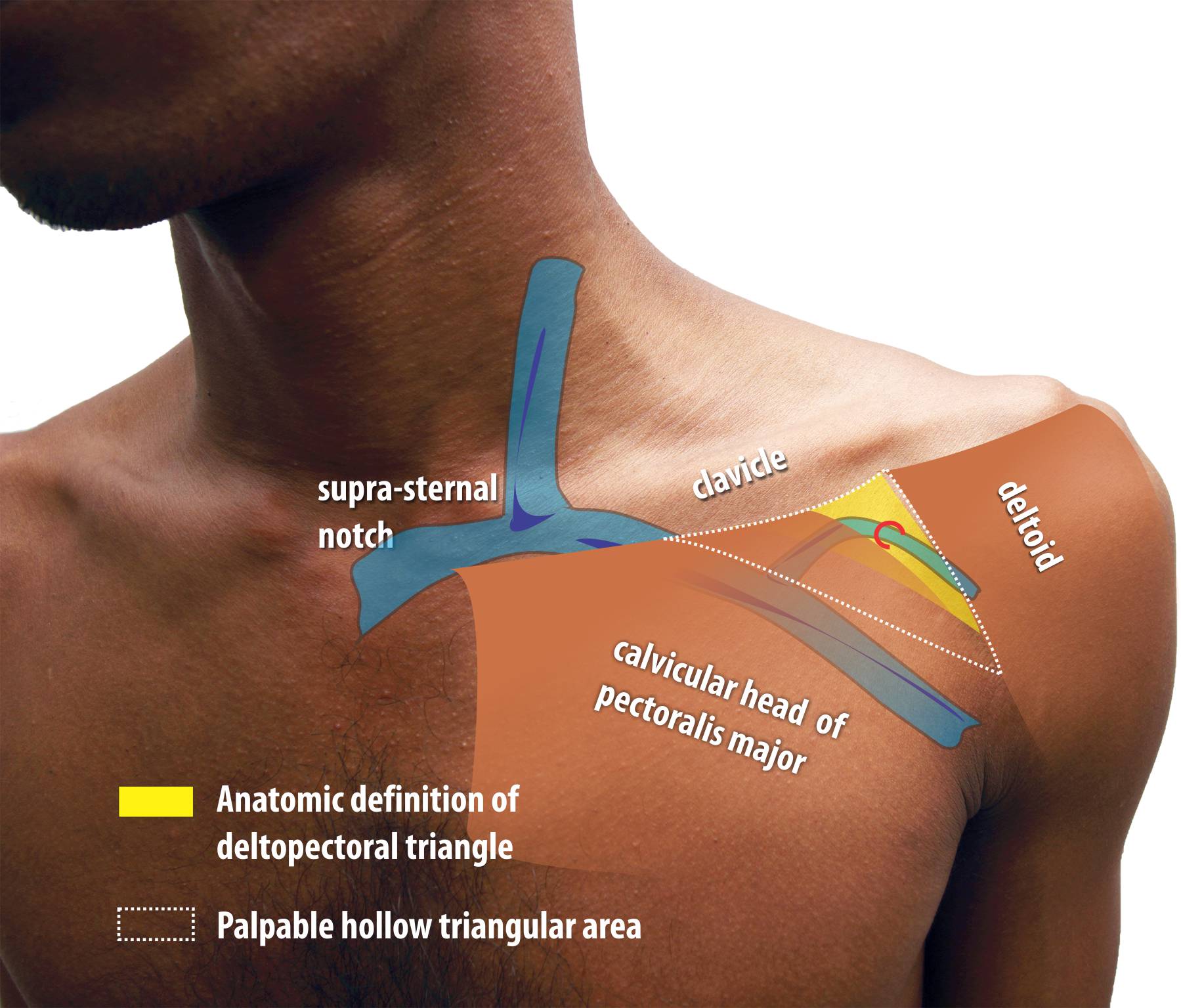
The deltopectoral triangle is a triangular depression formed between the clavicle above, lateral border of the pectoralis major medially and the medial border of the deltoid laterally. This narrow triangular area contains investing layers of the clavipectoral fascia and the cephalic vein on its roof which it pierces.
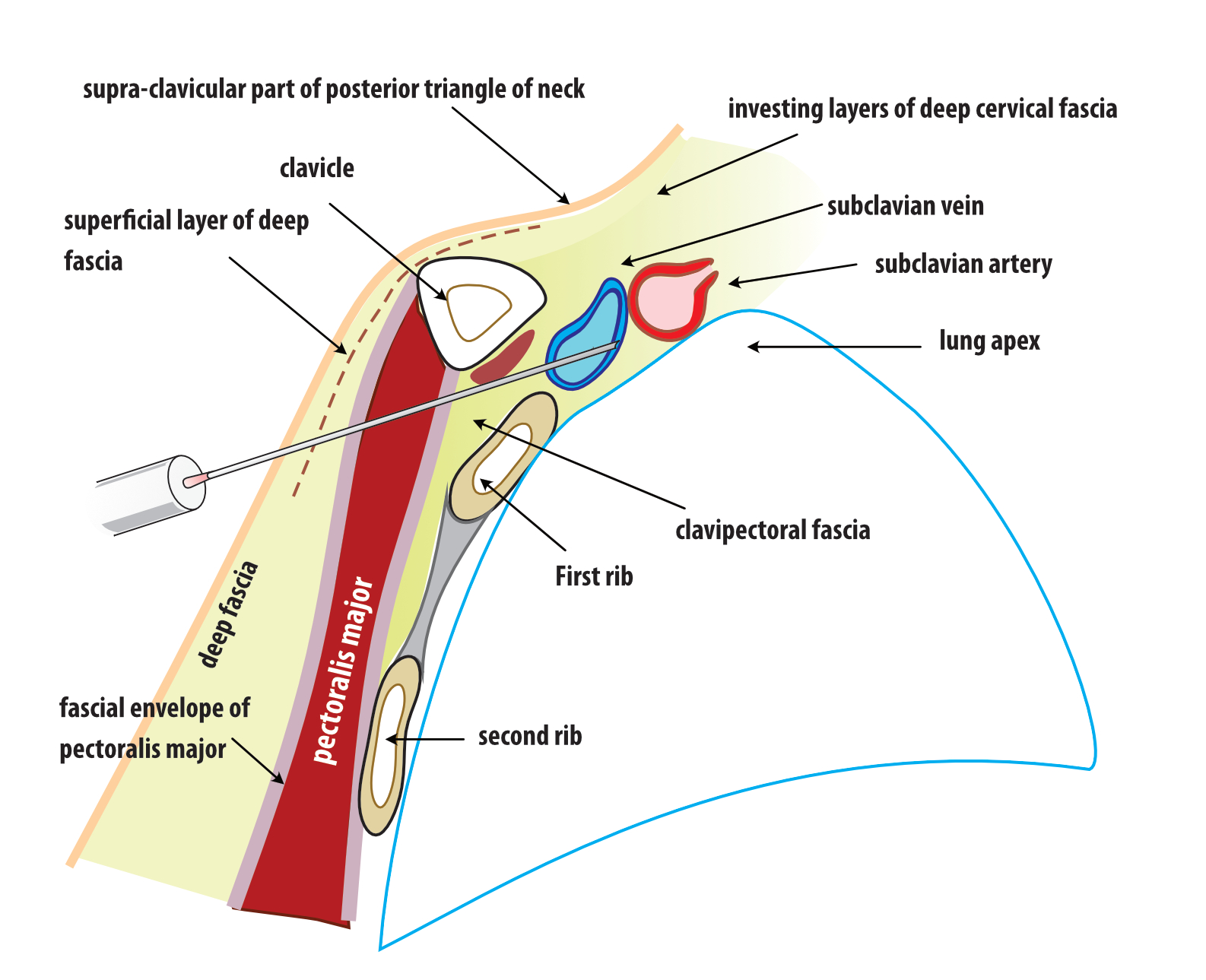
The investing layers of the clavipectoral fascia extend laterally along the vein and artery to blend with the axillary fascia.
The axillary vein which is the vein segment between the subclavian and the brachial vein is an extra-thoracic structure which lies deep to the pectroralis major muscle and is a component of the anterior wall of the axilla.
The subclavian vein lies anterior to the artery on the anterior aspect of the first rib when it crosses over it. medial to the first rib, the vein is considered an intra-thoracic structure. The upper limb drains to the central venous system by means of axillary vein which becomes the subclavian vein as it travels above the first rib towards the thoracic inlet.
The cephalic vein which drains the superficial lateral part of the upper limb lies within the lateral part part of deltopectoral triangle along the groove and dives deep through its floor to enter axillary vein which lies deep behind the pectoralis major muscle.
Figure : The Deltopectoral Region. Yellow colored zone corresponds to strict anatomic definition but the physically palpable triangular depression is of more practical relevance to punctured venous access. The cephalic vein lies on a grove just medial to the medal margin of deltoid and is sometimes marked by a skin crease. The cephalic vein pierces the fascia to enter the deeper aspect of the pecoralis major and enter the axillary vein
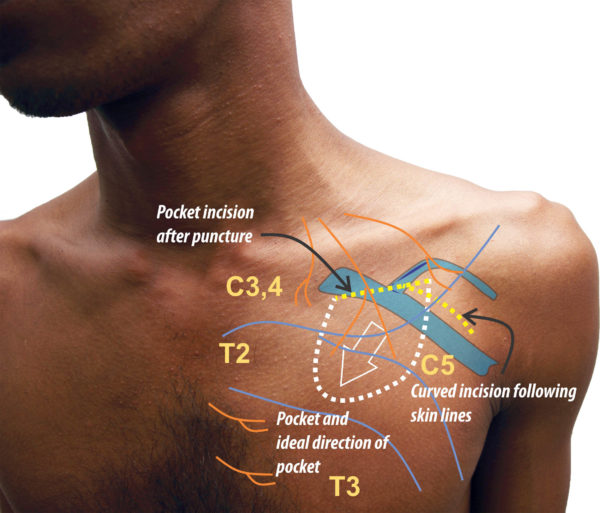
Figure : Schematic of Pocket location and Skin Incision. There are two broad ways of making an incision for the device pocket. An incision made parallel and about two finger-breadths below the mid-clavicle was is the authors’s initial method of choice. It gives good access to punctured venous access and placement of leads. The second method is the curved incision placed over the roof of the delto-pectoral groove confirming to Langers’ lines. This incision had its origin in facilitating cephalic cut-down as the former will not facilitate such – however this version is slightly more medial and inferior compared to the classic cutdown incision to hunt the vein. The author’s current preference is to use this incision – even for punctured access as it gives a superior cosmetic outcome compared to the prior incision. This incision is particularly suited for extra-thoracic subclavian (axillary) puncture access method. The only caveat is that if the access proves to be difficult and the needle needs to be more medial (subclavian position) this incision may need an extension medially. This is incision mandates meticulous local anaesthetic technique as the supra-clavicular nerves may not be fully blocked if the anaesthetic needle is not fully directed towards them. In either case the pocket is directed medially to avoid lateral erosion.
Soft Tissue
The soft tissue covering includes the skin, deep fascia (usually with two layers), clavipectoral fascia and the pectoralis major muscle.
The deep fascia is a network of fat and fibrous tissue which help support the skin on the chest wall and has two layers with an intervening fibrous separation which can sometimes be seen in patients. If present, this layer can be used for approximation of the superficial part of the pocket (more on pocket closure here : ) Rarely muscle fibers (platysma) may be visible in this layer and must not be confused as the pectoralis major muscle. Gentle blunt poking with a mosquito forceps will reveal that there is more fascia underneath this layer and it is not the true pectoralis major muscle.) This superficial part has more blood vessels compared to the deeper layer
The deep layer of the deep fascia is variable in thickness and mainly consists of fat – especially in females. The breast lies within a pocket formed by this layer and in females, the suspensory ligaments of the breast travel through this space. The breast may be encountered in creating pockets in young females (teenagers) when the device is large (e. g. ICD)
The pectoralis major muscle is covered by a thin but strong fascial layer – the clavipectoral fascia. Bulk of the fascia is actually deep to (behind) the muscle and it’s principle role is to give support to the structures of the axilla by enclosing the neurovascular structures that exit and enter the thoracic inlet. Fortunately for us pacemaker implanter’s, this fascial layer on the muscle is only loosely attached to the deep fascia. Therefor when one dissects up to the muscle and sees the fascial covering, its a matter of blunt finger dissection to create a pocket between the fascial envelope of the muscle and deep fascia.
The hiatus between the pectoralis major muscle and the deltoid – i. e. the deltopectoral groove is filled up by the calvipectoral fascia with deep fascia forming the roof. The cephalic vein traverses along the roof and pierces the clavipectoral fascia to enter the underside of the pectoralis major muscle and travels towards the axiallry vein to join it.
Figure : Schematic of pacemaker pocket and the relationship with the surrounding soft tissue (See text above for description)
Figure : Fibrous layer between the superficial part and the deep part of the deep fascia (in some patients, this layer may have fibers of the Platysma muscle)
Nerve supply
Sensory nerve supply for this area a supplied by three groups of cutaneous nerves. Understanding their course and distribution helps efficient administration of local anaesthesia
Supra-clavicular nerves of the cervical plexus : These fibers descend from the neck, superficial to the clavicle. These are the principle nerves which supply the skin of the operative region. As described later, adequate deep infiltration of local anesthesia along the proposed skin incision blocks these nerves and delivers a large field of anesthesia that is useful for creation of the pocket. The dermatome is C3
Lateral cutaneous nerves from the intercostal nerves : From T3 downwards, these pierce the lateral margin of the pectoralis major give branches which travel forward and backwards along the deep fascia superficial to the muscle. The anterior branches provide sensation to the infero-lateral area of our pacemaker pocket. T2’s cutaneous branch only provides the axilla via the intercostobrachial nerve. T1 has no cutaneous branches to the thorax.
Anterior cutaneous nerves from intercostal nerves : These are perforating termini of the intercostal nerves that exit at the anterior end of the intercostal space (near the sternal border). The pierce the pectoralis major muscle and reach the subcutaneous plane and provide the sensation to the medial aspect of our pacemaker pocket. The relevant dermatomes are T2 – T4
The hiatus between the pectoralis major muscle and the deltoid – i. e. the deltopectoral groove is filled up by the calvipectoral fascia with deep fascia forming the roof. The cephalic vein traverses along the roof and pierces the clavipectoral fascia to enter the underside of the pectoralis major muscle and travels towards the axiallry vein to join it.
Further Reading :