Tips and Tricks for difficult venous access
Troubleshooting – Venous Access
Troubleshooting in Venous Access
Although looks trivial, venous access is the most trickiest part of a pacemaker implantation. The biggest acute morbidity of a pacemaker implantation – a pneumothorax is related to punctured venous access and therefore its not surprising that a large number of centers still practice the method of venous cut-down !
Additionally, one must ensure that longevity of the lead and system are not compromised by a misplaced entry point (e.g. a very medial puncture)
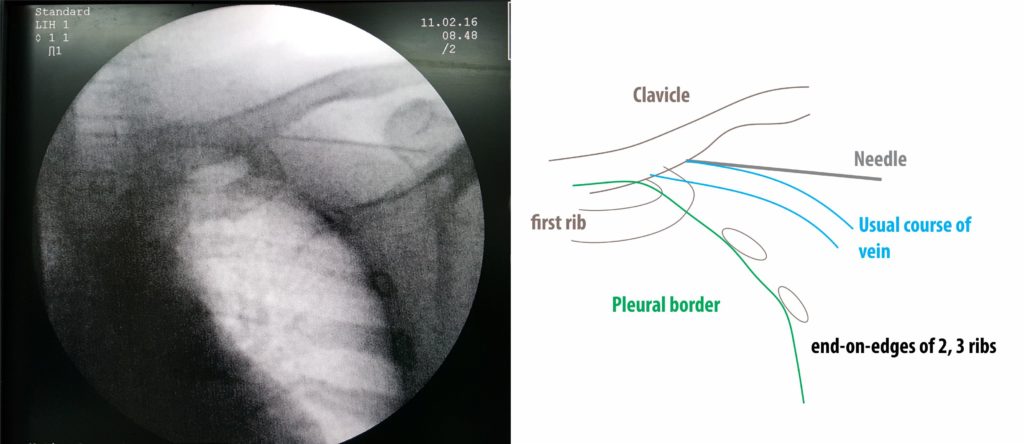
If no access is gained after few attempts, a venogram should be done to delineate the venous anatomy. Persisting on attempting without a visual anatomical clue increases the risk of penumothorax. This is especially true for implanters who are in their learning curve – doing a venogram trains the operator on the correct orientation.
The important points are to advance in fine steps with gentle suction and as soon as blood is seen to stop advancing and aspirate. (With experience, the operator will feel a characteristic giveaway when entering the vein). When advancement is done with fine steps, even in the event of a pleural breech one will not have advanced too much into the lung space thus minimizing depth of lung penetration (air would be aspirated if the lung substance was breached). The parietal pleura is very pain sensitive (via intercostal nerves) and our initial local anesthesia generally does not anesthetize this. Therefore if a giveaway occurs with sharp pain, immediately withdraw the needle as this may be a pleural breach. Soft tissue, vessels (and even the rib periosteum !!) are relatively pain insensitive.
Potential Issues in a difficult venous access
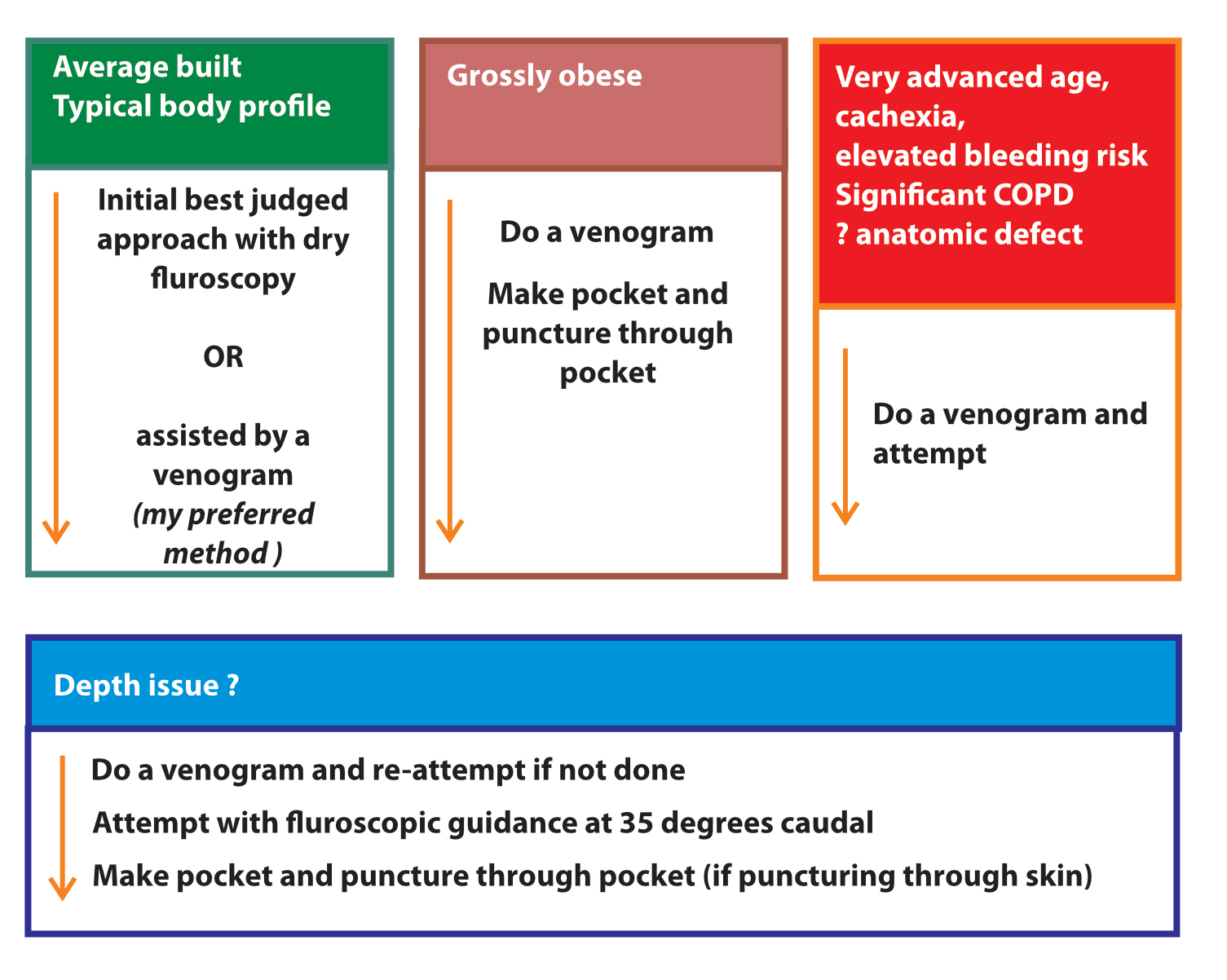
Wrap-up : Workflow guide for vein access
Figure : The venous puncture workflow cascade. With experience, the operator can get venous access easily. In a vast majority of patients, access succeeds in 1 to 3 attempts. The key is anticipating difficulty before attempting a puncture. Low BMI, female sex, COPD, age > 80, dual chamber device are risk factors(1) for a pneumothorax and a low threshold for radiologic aid (venography or ultrasound) should be the norm for these patients. Persisting without a radiologic aid is asking for trouble. Always try to access the axillary vein rather than the subclavian vein and if a venogram is done, use it to guide the punctures – especially in multi lead devices. (The role of the venogram is to guide the puncture at the best location – not to merely reassure the presence of the vein and attempt randomly!).
Note on venous cutdowns : The author has minimal experience in cutdowns (there had been no necessity for a cutdown in the recent past in author’s institution). However it may be the best option to chose in the hands of an experienced cut-downer when punctured access becomes difficult
Further Reading :